Every year, 15 million infants around the world are born too early and before completion of the 37th week of pregnancy¹. These children face substantial challenges that are more severe the earlier the child is born. The first challenge that they, their parents, and the hospital staff are facing is to keep the child alive¹.
Health challenges of premature birth
Preterm birth is the number one cause of child mortality and morbidity around the world¹. The earlier in a pregnancy infants are born, the less prepared their bodies are for the outside world and the more special care they need to stay alive¹. Preterm infants are at risk of developing disabilities that will affect their entire lives. The extent strongly depends on how early they were born, what medical challenges they have to overcome, the quality of care they received during and around birth, and the period that follows¹.
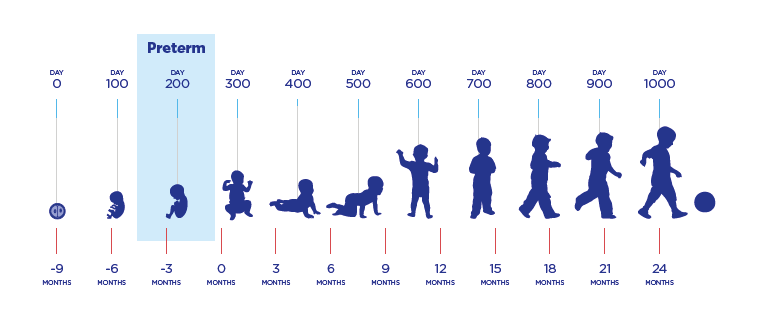
We believe the right nutrition in the first 1,000 days has the power to influence preterm infants’ health for life. Nutrition in the early developmental phase plays an important role in ensuring optimal development of all organ systems and their ability to adapt to environmental challenges to ensure lifelong health.

The third or last trimester of pregnancy is a critical phase for development and growth. This trimester begins at 27 weeks until the child’s due date at 40 weeks. During this last trimester, the fetus experiences a period of rapid physical growth together with a marked increase in the functional capacity of the developing organs²⁻⁴.
Achieving adequate growth velocity, a key challenge for long term health
The aim for preterm infants is to grow and develop at a similar pace outside of the mother’s womb as they would during the same period inside the womb⁵`⁶. Achieving appropriate growth and nutrient accretion is often difficult because of the special needs of the preterm infant as a result of metabolic and gastrointestinal immaturity ⁵⁻⁷.
Key challenges of premature infants are:
- Need for a high growth velocity versus difficulties of enteral food intake⁵`⁶
- Gastrointestinal & metabolic immaturity⁵
- Immature /compromised immune system⁷
- Use of antibiotics leading to delayed colonisation and compromised microbiota development⁷
- Sensitive phase of brain development⁸
High nutrient requirement vs compromised nutritional intake
The intrauterine growth rate desired for preterm infants can be three to five times higher than that at term ⁵`⁹ and therefore the nutritional requirements are increased ⁵`⁶`⁹.
However, a limited feeding ability together with a limited stomach volume present a challenge to meet these nutritional requirements enterally ¹`⁵`⁶. This is further compounded by the immature ability to adequately digest and absorb (some) nutrients, limited nutrient reserves and low body fat stores ⁵`⁶.
Compromised gut barrier and immune health
Infections, necrotising enterocolitis and sepsis compromise survival and negatively affect the growth rate of the infant ⁷`¹⁰. Preterm infants are at increased risk of infections because of medical interventions (e.g. feeding intravenously), the hospital environment with potential pathogens, and an immature gut barrier and immune system ⁷. Intestinal microbiota play a role in our immune defence ⁷`¹¹. Prophylactic use of antibiotics delay colonisation and thereby contribute to the increased infection risk and potentially to subsequent growth deficits ⁷`¹¹.

A sensitive phase of brain development
The last trimester up to 2 years of age is a sensitive phase of brain development ⁸. If growth deficits occur, functional organ development is compromised — particularly brain development — with potentially severe long-term effects ⁸`¹²`¹³.

40 years of early life science
Nutricia Early Life Nutrition has over 40 years of breast milk expertise with a dedicated team of around 250 specialist scientists collaborating with hospitals, laboratories and universities worldwide to ensure we’re leaders in this field.
Our careline
Our free healthcare professional helpline is open from 8am to 8pm, Monday to Friday. Just phone 0800 996 1234 for expert advice on infant feeding and nutrition, including common infant feeding problems such as cows’ milk allergy, colic, constipation and reflux.
IMPORTANT NOTICE: Breastfeeding is best for babies. Infant formula is suitable from birth when babies are not breastfed. Follow-on milk is only for babies over 6 months, as part of a mixed diet and should not be used as a breastmilk substitute before 6 months. We advise that all formula milks including the decision to start weaning should be made on the advice of a doctor, midwife, health visitor, public health nurse, dietitian, pharmacist or other professional responsible for maternal and child care. Foods for special medical purposes should only be used under medical supervision. May be suitable for use as the sole source of nutrition for infants from birth, and/or as part of a balanced diet from 6–12 months. Refer to label for details.



